Die Patella, allgemein als Kniescheibe bekannt, ist ein Sesambein, das aus der Quadrizepssehne entsteht und gleichzeitig das größte Sesambein des Körpers ist. Sie ist flach und hirseförmig, liegt unter der Haut und ist leicht zu ertasten. Der Knochen ist oben breit und spitz zulaufend, mit einer rauen Vorderseite und einer glatten Rückseite. Er ist beweglich und schützt das Kniegelenk. Die Rückseite der Patella ist glatt und mit Knorpel überzogen und verbindet sich mit der Kniescheibenfläche des Oberschenkelknochens. Die Vorderseite ist rau, und die Quadrizepssehne verläuft durch sie hindurch.
Die Chondromalazie der Patella ist eine häufige Kniegelenkserkrankung. Früher trat sie vorwiegend bei Menschen mittleren und höheren Alters auf. Mit der zunehmenden Beliebtheit von Sport und Fitness ist die Erkrankung heute auch bei jungen Menschen weit verbreitet.
I. Was ist die wahre Bedeutung und Ursache der Chondromalacia patellae?
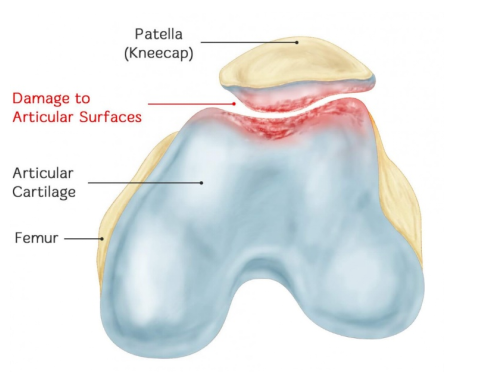
Die Chondromalacia patellae (CMP) ist eine patellofemorale Arthrose, die durch chronische Schädigung der Kniescheibenknorpeloberfläche verursacht wird. Dies führt zu Knorpelschwellungen, Rissen, Brüchen, Erosionen und Ablösung des Knorpels. Schließlich ist auch der Knorpel des gegenüberliegenden Oberschenkelknochens betroffen. CMP bedeutet also: Es kommt zu einer pathologischen Veränderung der Kniescheibenknorpelerweichung, die mit Symptomen wie Kniescheibenschmerzen, Kniescheibengeräuschen und Atrophie des Quadrizepsmuskels einhergeht.
Da Gelenkknorpel keine Nervenversorgung besitzt, ist der Schmerzmechanismus bei Chondromalazie noch nicht vollständig geklärt. Die Chondromalazie entsteht durch das Zusammenwirken mehrerer Faktoren. Verschiedene Faktoren, die den Druck im Patellofemoralgelenk verändern, sind externe Ursachen, während Autoimmunreaktionen, Knorpeldystrophie und Veränderungen des intraossären Drucks interne Ursachen der Chondromalazie patellae darstellen.
II. Das bedeutendste Merkmal der Chondromalacia patellae sind die spezifischen pathologischen Veränderungen. Wie wird die Chondromalacia patellae also aus der Perspektive der pathologischen Veränderungen eingeteilt?
Insall beschrieb vier pathologische Stadien der CMP: Stadium I ist die Knorpelerweichung durch Ödeme, Stadium II ist auf Risse im erweichten Bereich zurückzuführen, Stadium III ist die Fragmentierung des Gelenkknorpels; Stadium IV bezieht sich auf die erosiven Veränderungen der Osteoarthritis und die Freilegung des subchondralen Knochens auf der Gelenkfläche.
Das Outerbridge-Klassifikationssystem eignet sich am besten zur Beurteilung von Knorpelschäden an der Kniescheibe unter direkter Sicht oder Arthroskopie. Das Outerbridge-Klassifikationssystem ist wie folgt:
Grad I: Lediglich der Gelenkknorpel ist erweicht (geschlossene Knorpelerweichung). Zur Beurteilung ist in der Regel eine taktile Untersuchung mit einer Sonde oder einem anderen Instrument erforderlich.
Grad II: Teildickende Defekte mit einem Durchmesser von höchstens 1,3 cm (0,5 Zoll) oder die den subchondralen Knochen nicht erreichen.
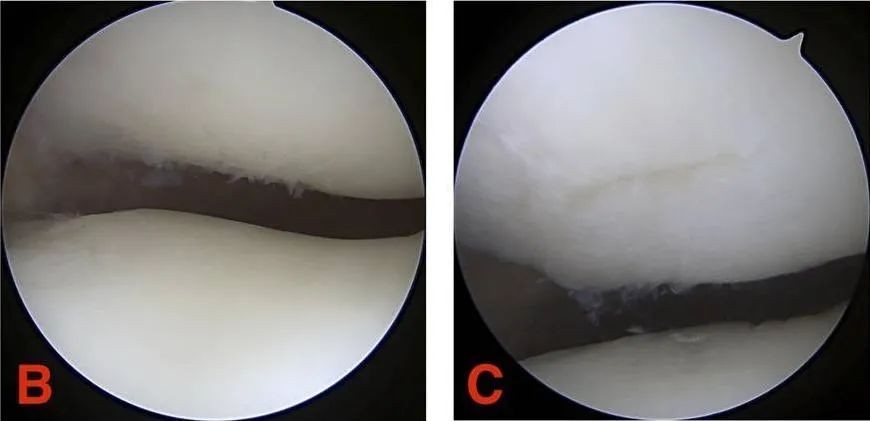
Grad III: Der Knorpelriss hat einen Durchmesser von mehr als 1,3 cm (1/2 Zoll) und reicht bis zum subchondralen Knochen.

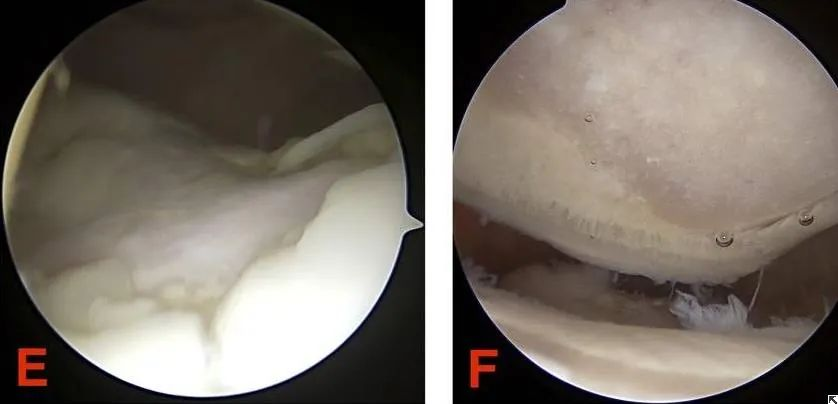
Grad IV: Freilegung des subchondralen Knochens.
III. Sowohl die Pathologie als auch die Graduierung spiegeln das Wesen der Chondromalacia patellae wider. Was sind also die aussagekräftigsten Anzeichen und Untersuchungen zur Diagnose der Chondromalacia patellae?
Die Diagnose basiert hauptsächlich auf Schmerzen hinter der Kniescheibe, die durch den Patellareibtest und den Einbein-Kniebeugetest ausgelöst werden. Es gilt abzuklären, ob eine kombinierte Meniskusverletzung und traumatische Arthritis vorliegen. Allerdings besteht kein Zusammenhang zwischen dem Schweregrad der Chondromalazie der Kniescheibe und den klinischen Symptomen des vorderen Knieschmerzsyndroms. Die MRT ist eine genauere Diagnosemethode.
Das häufigste Symptom ist ein dumpfer Schmerz hinter der Kniescheibe und im Knieinneren, der sich nach Anstrengung oder beim Treppensteigen verschlimmert.
Die körperliche Untersuchung zeigt eine deutliche Druckempfindlichkeit der Kniescheibe, des peripatellaren Bereichs, des Kniescheibenrandes und der hinteren Kniescheibe. Diese kann von Gleitschmerzen und Reibungsgeräuschen der Kniescheibe begleitet sein. Es können Gelenkergüsse und eine Atrophie des Quadrizepsmuskels vorliegen. In schweren Fällen sind Kniebeugung und -streckung eingeschränkt, und der Patient kann nicht auf einem Bein stehen. Beim Kompressionstest der Kniescheibe treten starke Schmerzen hinter der Kniescheibe auf, was auf eine Knorpelschädigung der Kniescheibe hinweist und diagnostisch relevant ist. Der Apprehensionstest und der Kniebeugetest sind häufig positiv. Übersteigt der Bewegungsumfang der Kniescheibe bei einer Kniebeugung von 20° bis 30° ein Viertel ihres Querdurchmessers, deutet dies auf eine Kniescheibenluxation hin. Die Messung des Q-Winkels bei 90° Kniebeugung kann eine abnorme Bewegungsbahn der Kniescheibe widerspiegeln.
Die zuverlässigste ergänzende Untersuchungsmethode ist die MRT, die die Arthroskopie zunehmend abgelöst hat und sich zu einem nicht-invasiven und zuverlässigen Verfahren zur Beurteilung der chronischen idiopathischen Arthritis (CMI) entwickelt hat. Bildgebende Verfahren konzentrieren sich hauptsächlich auf folgende Parameter: Patellahöhe (Caton-Index, PH), Trochleawinkel (FTA), laterales Oberflächenverhältnis der Trochlea femoris (SLFR), Patellasitzwinkel (PCA) und Patellaneigungswinkel (PTA). PH, PCA und PTA sind dabei zuverlässige Kniegelenksparameter für die ergänzende Diagnose einer beginnenden CMI.
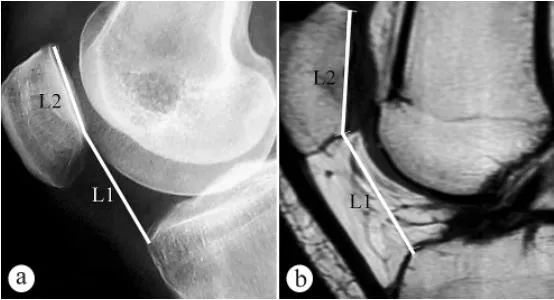
Zur Messung der Patellahöhe (Caton-Index, PH) wurden Röntgenaufnahmen und MRT-Bilder verwendet: a. Axiale Röntgenaufnahme in stehender Position unter Belastung mit 30° gebeugtem Knie, b. MRT-Aufnahme in Position mit 30° gebeugtem Knie. L1 ist der Patellainklinationswinkel, d. h. der Abstand zwischen dem tiefsten Punkt der patellofemoralen Gelenkfläche und dem anterioren oberen Winkel der Tibiaplateaukontur, L2 ist die Länge der patellofemoralen Gelenkfläche, und der Caton-Index berechnet sich als L1/L2.
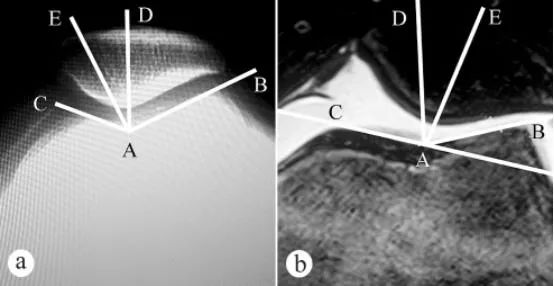
Der Femurtrochleawinkel und der Patellapasswinkel (PCA) wurden mittels Röntgen und MRT gemessen: a. Axiale Röntgenaufnahme bei 30° Knieflexion in gewichtsbelasteter Stehposition; b. MRT bei 30° Knieflexion. Der Femurtrochleawinkel wird durch zwei Linien bestimmt: den tiefsten Punkt A der Femurtrochlea, den höchsten Punkt C der medialen Trochlea-Gelenkfläche und den höchsten Punkt B der lateralen Trochlea-Gelenkfläche. ∠BAC ist der Femurtrochleawinkel. Dieser wurde auf dem axialen Patellabild eingezeichnet, anschließend die Winkelhalbierende AD von ∠BAC. Von Punkt A der Femurtrochlea als Ursprung wurde dann eine Gerade AE durch den tiefsten Punkt E des Patellakamms gezogen. Der Winkel zwischen den Geraden AD und AE (∠DAE) ist der Patellapasswinkel.
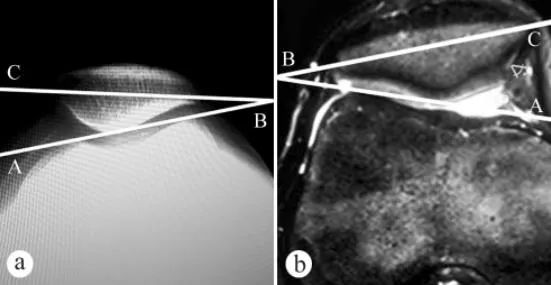
Zur Messung des Patellaneigungswinkels (PTA) wurden Röntgenaufnahmen und MRT-Bilder verwendet: a. Axiale Röntgenaufnahme in stehender, belasteter Position mit 30° gebeugtem Knie, b. MRT-Aufnahme in dieser Position mit 30° gebeugtem Knie. Der Patellaneigungswinkel ist der Winkel zwischen der Verbindungslinie der höchsten Punkte des medialen und lateralen Femurkondylus und der Querachse der Patella, d. h. ∠ABC.
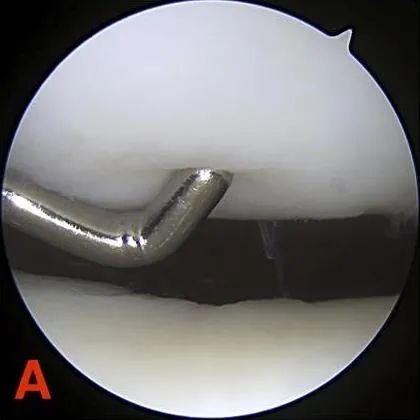
Röntgenaufnahmen sind in frühen Stadien der CMP (Chondromalazie der Patella) schwierig zu diagnostizieren, bis in fortgeschrittenen Stadien ein ausgeprägter Knorpelverlust, eine Gelenkspaltverengung sowie eine damit einhergehende subchondrale Knochensklerose und zystische Veränderungen sichtbar werden. Die Arthroskopie ermöglicht eine zuverlässige Diagnose, da sie eine exzellente Visualisierung des Patellofemoralgelenks bietet. Allerdings besteht kein eindeutiger Zusammenhang zwischen dem Schweregrad der Patellachondromalazie und dem Ausmaß der Symptome. Daher sollten diese Symptome keine Indikation für eine Arthroskopie darstellen. Auch die Arthrographie wird als invasives Diagnoseverfahren in der Regel erst in fortgeschrittenen Stadien der Erkrankung eingesetzt. Die MRT ist ein nicht-invasives Diagnoseverfahren, das die einzigartige Möglichkeit bietet, Knorpelschäden sowie interne Knorpelveränderungen zu erkennen, bevor ein morphologischer Knorpelverlust mit bloßem Auge sichtbar ist.
IV. Die Chondromalacia patellae kann reversibel sein oder zu einer Patellofemoralarthrose fortschreiten. Eine wirksame konservative Therapie sollte im Frühstadium der Erkrankung umgehend eingeleitet werden. Was umfasst diese konservative Therapie?
Es gilt allgemein als erwiesen, dass sich der Kniescheibenknorpel im Frühstadium (Stadium I bis II) noch regenerieren kann und eine wirksame nicht-operative Behandlung erfolgen sollte. Diese umfasst hauptsächlich Schonung oder körperliche Aktivitätseinschränkung sowie gegebenenfalls die Einnahme von nichtsteroidalen Antirheumatika. Zusätzlich sollten Patienten unter Anleitung eines Physiotherapeuten Übungen zur Kräftigung der Oberschenkelmuskulatur und zur Verbesserung der Kniegelenksstabilität durchführen.
Es ist zu beachten, dass während der Ruhigstellung in der Regel Knieorthesen oder Kniebandagen getragen werden und eine Gipsfixierung möglichst vermieden wird, da diese leicht zu einer Inaktivitätsverletzung des Gelenkknorpels führen kann; obwohl eine Blockadetherapie die Symptome lindern kann, sollten Hormone nicht oder nur sparsam eingesetzt werden, da sie die Synthese von Glykoproteinen und Kollagen hemmen und die Knorpelreparatur beeinträchtigen; wenn sich Gelenkschwellung und Schmerzen plötzlich verschlimmern, können Eiskompressen angewendet werden, und Physiotherapie und warme Kompressen können nach 48 Stunden angewendet werden.
V. Bei Patienten im fortgeschrittenen Stadium ist die Regenerationsfähigkeit des Gelenkknorpels gering, sodass eine konservative Behandlung oft wirkungslos ist und ein chirurgischer Eingriff erforderlich ist. Was umfasst ein chirurgischer Eingriff?
Indikationen für eine Operation sind: Nach mehrmonatiger streng konservativer Therapie bestehen weiterhin Schmerzen im Bereich der Kniescheibe; bei angeborener oder erworbener Deformität kann eine operative Behandlung erwogen werden. Bei einem Knorpelschaden vom Typ Outerbridge III-IV kann der Defekt nicht mehr durch echten Gelenkknorpel aufgefüllt werden. In diesem Fall reicht eine einfache Abtragung des geschädigten Knorpelbereichs bei gleichzeitiger chronischer Überlastung nicht aus, um den Prozess der Gelenkflächendegeneration aufzuhalten.
Zu den chirurgischen Methoden gehören:
(1) Die Arthroskopie ist eine effektive Methode zur Diagnose und Behandlung der Chondromalacia patellae. Sie ermöglicht die direkte Beobachtung der Knorpeloberflächenveränderungen unter dem Mikroskop. In leichten Fällen können kleinere Erosionsherde am Kniescheibenknorpel abgetragen werden, um die Regeneration zu fördern.

(2) Anhebung des lateralen Femurkondylus; (3) Resektion der Patellaknorpeloberfläche. Dieser Eingriff wird bei Patienten mit geringfügigen Knorpelschäden durchgeführt, um die Knorpelreparatur zu fördern; (4) eine Patellaresektion wird bei Patienten mit schweren Schäden an der Patellaknorpeloberfläche durchgeführt.
Veröffentlichungsdatum: 15. November 2024










